Contraception and the Menstrual Cycle: Science-Backed Guidance
Contraception and the Menstrual Cycle: Science-Backed Guidance
Introduction
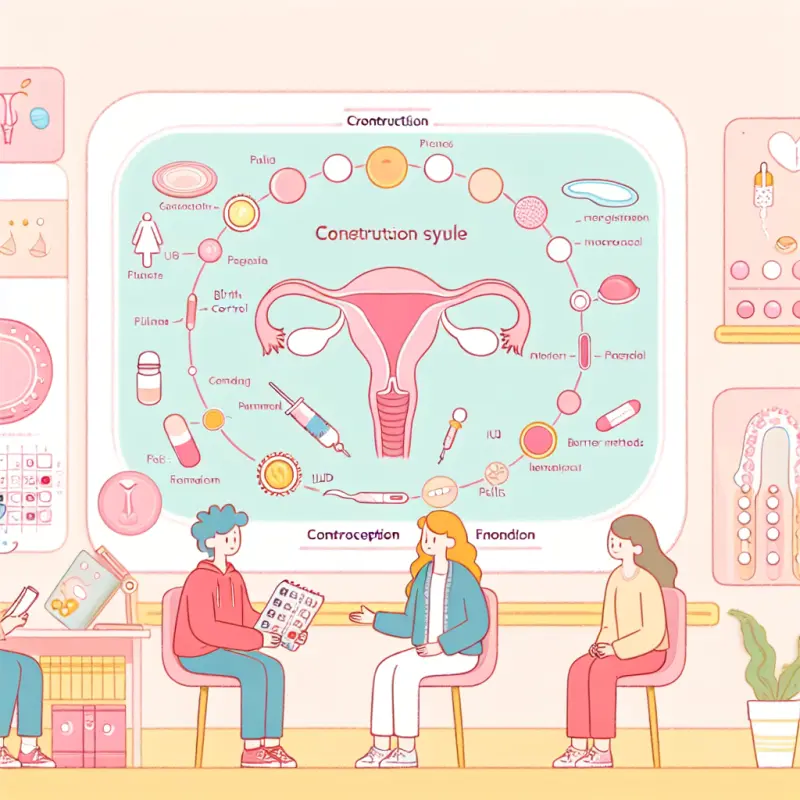
The menstrual cycle is a natural, intricate process that plays a crucial role in women's reproductive health. Understanding this cycle is essential when discussing contraception, as it can affect the choice, effectiveness, and side effects of various contraceptive methods. With numerous options available, ranging from hormonal to non-hormonal methods, choosing the right form of contraception can be daunting. This article delves into the science behind the menstrual cycle and contraception, providing guidance to help individuals make informed decisions.
Understanding the Menstrual Cycle
To comprehend how contraception interacts with the menstrual cycle, it is critical first to understand the cycle itself. The menstrual cycle is typically divided into four phases: menstruation, the follicular phase, ovulation, and the luteal phase.
1. Menstruation
- Duration: Usually lasts 3-7 days.
- Process: During menstruation, the uterine lining, also known as the endometrium, sheds, resulting in menstrual bleeding.
- Hormonal Changes: Low levels of estrogen and progesterone trigger the shedding of the uterine lining.
2. Follicular Phase
- Duration: Starts on the first day of menstruation and lasts until ovulation (about 14 days in a 28-day cycle).
- Process: The pituitary gland releases follicle-stimulating hormone (FSH), leading to the growth of ovarian follicles. One follicle becomes dominant and matures into an egg.
- Hormonal Changes: Estrogen levels begin to rise, thickening the uterine lining in preparation for a potential pregnancy.
3. Ovulation
- Duration: Occurs mid-cycle, around day 14 in a 28-day cycle.
- Process: A surge in luteinizing hormone (LH) triggers the release of the mature egg from the ovary.
- Fertility Window: This is the most fertile phase of the cycle, lasting about 12-24 hours. However, sperm can survive in the female reproductive tract for up to five days, extending the fertile window.
4. Luteal Phase
- Duration: Lasts from ovulation until the start of menstruation (about 14 days).
- Process: The ruptured follicle transforms into the corpus luteum, producing progesterone.
- Hormonal Changes: Progesterone maintains the uterine lining. If pregnancy does not occur, progesterone and estrogen levels drop, leading to menstruation.
Contraceptive Methods and Their Interaction with the Menstrual Cycle
Contraceptive methods can be broadly categorized into hormonal and non-hormonal methods. Each interacts differently with the menstrual cycle, affecting its phases and hormonal balance.
Hormonal Contraceptives
Hormonal contraceptives are designed to manipulate the menstrual cycle to prevent pregnancy. They can be further divided into combined hormonal contraceptives and progestin-only contraceptives.
Combined Hormonal Contraceptives (CHCs)
These contraceptives contain both estrogen and progestin, which work together to prevent ovulation, thicken cervical mucus, and thin the uterine lining.
- Oral Contraceptive Pills (OCPs): Taken daily, these pills maintain consistent hormone levels to suppress ovulation.
- Contraceptive Patch: Applied weekly, it delivers hormones through the skin.
- Vaginal Ring: Inserted monthly, it releases hormones directly into the bloodstream.
Interaction with the Menstrual Cycle:
- Suppression of Ovulation: By maintaining steady hormone levels, CHCs prevent the LH surge necessary for ovulation.
- Alteration of Menstruation: Menstrual bleeding while on CHCs is often lighter and more regular, referred to as withdrawal bleeding.
- Cycle Regulation: CHCs can stabilize irregular menstrual cycles and reduce symptoms such as acne and menstrual cramps.
Progestin-Only Contraceptives
These contraceptives contain only progestin, making them suitable for individuals who cannot take estrogen.
- Progestin-Only Pills (POPs): Taken daily, these pills primarily thicken cervical mucus and may suppress ovulation in some users.
- Injectable Contraceptives: Administered every three months, these injections provide long-term suppression of ovulation.
- Implants: Inserted under the skin, they provide up to three years of contraception by releasing progestin.
- Hormonal IUDs: Inserted into the uterus, they release progestin locally, lasting between 3-6 years.
Interaction with the Menstrual Cycle:
- Variable Effects on Ovulation: While some progestin-only methods consistently suppress ovulation, others may not, leading to variable cycle effects.
- Menstrual Changes: Users may experience irregular bleeding, spotting, or amenorrhea (absence of menstruation).
Non-Hormonal Contraceptives
Non-hormonal methods do not interfere with the menstrual cycle's hormonal balance. They prevent pregnancy through physical barriers or behavioral methods.
Barrier Methods
- Condoms: Male and female condoms prevent sperm from entering the uterus.
- Diaphragms and Cervical Caps: Placed over the cervix to block sperm.
Interaction with the Menstrual Cycle:
- No Hormonal Interference: These methods do not affect menstrual hormones or cycle regularity.
- Protection Against STIs: Condoms provide additional protection against sexually transmitted infections.
Copper Intrauterine Device (IUD)
- Mechanism: The copper IUD is a small, T-shaped device inserted into the uterus. It releases copper ions, which are toxic to sperm, impairing their motility and preventing fertilization. The copper also creates an environment in the uterus that is inhospitable to implantation.
- Duration: Provides long-term contraception, typically effective for 5 to 10 years depending on the specific device.
- Effect on Menstrual Cycle: The copper IUD does not contain hormones and therefore does not suppress ovulation or alter the body's natural hormonal cycle. However, some users may experience heavier, longer, or more painful periods, especially in the first few months after insertion. Over time, these side effects may lessen for some individuals.
- Fertility After Removal: Fertility returns quickly after the device is removed.
Fertility Awareness-Based Methods
Fertility awareness methods (FAMs) involve tracking the menstrual cycle to identify fertile days and abstaining from unprotected sex or using barrier methods during that time.
- Types: Calendar method, basal body temperature tracking, cervical mucus monitoring, and symptothermal method (combining several indicators).
- Effect on Menstrual Cycle: These methods do not alter the menstrual cycle or hormone levels. They require a good understanding of one’s cycle and consistent, accurate tracking.
- Considerations: Effectiveness depends on correct and consistent use. These methods do not protect against sexually transmitted infections (STIs).
Emergency Contraception
Emergency contraception can be used after unprotected sex to prevent pregnancy.
- Types: Emergency contraceptive pills (ECPs) and the copper IUD (when inserted within 5 days after unprotected intercourse).
- Effect on Menstrual Cycle: ECPs may temporarily alter the timing of the next period, causing it to come earlier or later than expected. The copper IUD, when used as emergency contraception, does not affect the cycle beyond its usual effects as a long-term contraceptive.
Choosing the Right Contraceptive Method
The best contraceptive method depends on individual health, lifestyle, preferences, and reproductive goals. Considerations include:
- Health Conditions: Some methods may not be suitable for individuals with certain health conditions.
- Menstrual Symptoms: Hormonal methods can help manage symptoms like heavy bleeding or cramps, while non-hormonal methods avoid hormonal side effects.
- Convenience and Commitment: Some methods require daily attention, while others are long-acting or used only at the time of intercourse.
- Desire for Future Fertility: Most methods are reversible, but some (like sterilization) are permanent.
Consulting with a healthcare provider can help determine the most appropriate and effective method for your needs.
Conclusion
Understanding how different contraceptive methods interact with the menstrual cycle empowers individuals to make informed choices about their reproductive health. Whether you prefer hormonal, non-hormonal, or behavioral methods, there are options to suit a variety of needs and lifestyles. If you have questions or concerns about contraception or your menstrual cycle, speak with a healthcare professional for personalized guidance.